


































To make available to every individual, the best quality of health care treatments and solutions irrespective of their awareness, knowledge and financial status.


*Includes data of all our locations
Being one of the best eye hospital Chain in India, ASG Eye Hospital provides state-of-the-art Ophthalmology services in Cataract, Retina, Squint, Glaucoma, Cornea, Oculoplasty
All our doctors are available 24×7 at respective locations
500+ Eye specialists out of which 250+ are alumni of premier institutes like All India Institute of Medical Sciences (New Delhi), Sankara Nethralaya, LV Prasad & Aravind Eye Institute

PHACO, CORNEA & REFRACTIV...
View Profile
PHACO, CORNEA, GLAUCOMA...
View ProfileASG provides complete eye care services by combining exceptional knowledge and experience with the latest technology in ophthalmology. Explore the details of our expertise in ocular conditions like cataracts, glaucoma, refractive errors, corneal diseases, neuro-ophthalmology, pediatric ophthalmology, squint, and others.

This condition is one of the leading causes of blindness in people with diabetes. It is a serious eye condition that can occur in individuals with diabetes. It is caused by damage to the blood vess...
Read More
we have a dedicated neuro-ophthalmology department that specializes in the diagnosis and treatment of conditions that affect the visual system and the brain. Neuro-ophthalmology is a subspecialty o...
Read More

Oculoplasty, also known as oculoplastic surgery or ophthalmic plastic surgery, is a specialized branch of ophthalmology that focuses on the diagnosis and treatment of disorders affecting the structures around the eyes, including the eyelids, tear ...
Read More
Pediatric ophthalmology is a subspecialty of ophthalmology that focuses on the diagnosis and treatment of eye problems in children. A pediatric ophthalmologist is a medical doctor who has completed specialized training in ...
Read More

Refractive surgeries are elective procedures chosen by
individuals seeking to correct their refractive errors and reduce
their dependence on glasses or contact lenses.
... Read More

Our Retina Specialists are highly skilled in diagnosing and treating a wide range of conditions related to the retina, which is the delicate, light-sensitive tissue at the back of the eye. With advanced diagnostic tools and state-of-the-art treatm...
Read More
Q-LASIK, also known as Quick LASIK is an innovative and minimally invasive procedure designed to correct refractive errors in the eye, such as myopia (nearsightedness), hyperopia (farsightedness), and astigmatism. The technique employs advan...
Read More

Recently I have been operated for my Right Eye Surgery which was Performed by well known & expert Dr. Sean S Da Silva & the surgery was done successfu...

It was a great experience. The people were helpful and extremely professional. Strongly recommend this hospital to everyone...

My son mast Aarav rajoriya squint operation done by Dr Ganesh pillay at ASG hospital Bhopal. He is fine now. Dr Ganesh is doing excellent. We happy an...
Very good service. Helping , supporting and caring staff. Frank conversation. Good experience. We will definitely prefer this hospital for eye check u...
*includes data of all our locations
ASG Eye Hospital has provided comprehensive ophthalmic care for patients since 2005. Our skilled surgeons and staff strive to improve and preserve vision. We treat more than 50,000 patients a year. We ranked consistently among the best eye hospitals in India. Our team comprises some of India’s top eye doctors and surgeons. As a leading eye care center, we stand out as one of the top eye hospitals in India. Experience unparalleled eye care at ASG, the best eye hospital in India.
Expertise and Reputation - ASG Eye Hospital is one of the top eye hospitals in India and is known for its best-in-class eye care services. It has a long history of delivering exceptional ophthalmic services. Experienced doctors- Our team comprises the best eye doctors in India, dedicated to providing the best-in-class care and protecting your eye health.
Advanced Technology - As one of the biggest eye hospitals in India, we boast state-of-the-art facilities and cutting-edge technology to provide complete eye care services under one roof.
Specialization - we focus exclusively on eye care, making it a specialized hospital that offers a comprehensive range of services, from routine eye check-ups to advanced surgical procedures. Our eye doctors and surgeons provide a full range of primary and subspecialty eye care for enhancing and protecting vision involving primary eye care services, cataract, cornea, glaucoma, neuro-ophthalmology, oculoplasty, refractive surgery, retina, and other emergency eye care treatment.
Patient-Centric Care- the surgeons and staff at ASG Eye Hospital often prioritize personalized treatment plans considering each patient's unique needs and preferences.
Best-in-Class Infrastructure - We offer state-of-the-art facilities to our doctors by which they can perform complex surgeries with ease. At ASG Eye Hospital, we prioritize patient safety and efficient recovery. If you are looking for the most famous eye hospital in India, ASG is the right choice. Book an appointment today and take your first step towards the best eye surgery hospital in India. Our user-friendly online booking system makes it easy and convenient.
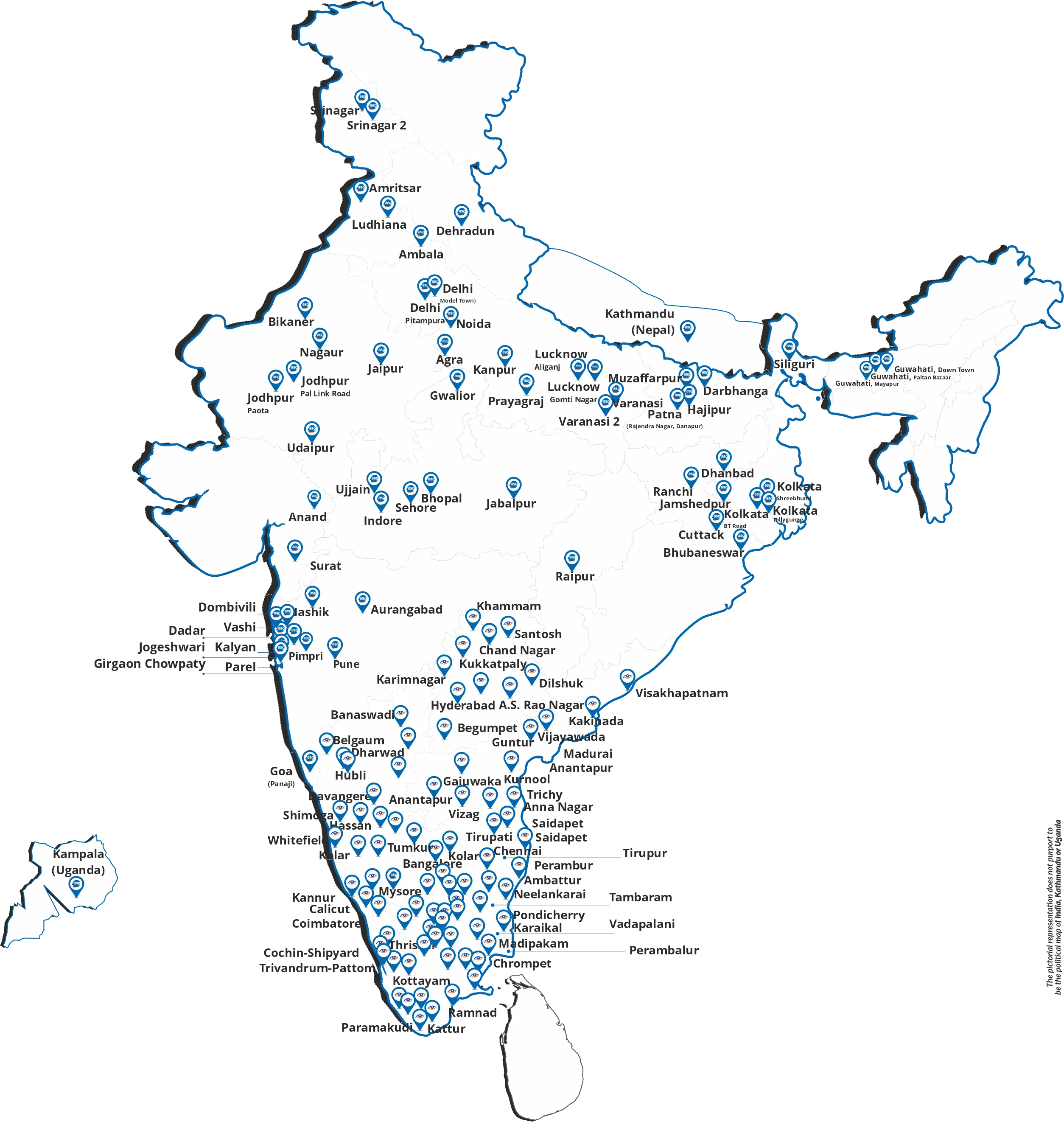
ASG Eye Hospital is a leading eye care provider with a network of state-of-the-art facilities across India. Our commitment to excellence in eye care makes us a preferred choice for patients seeking high-quality treatment and services.
ASG Eye Hospital is identified as one of the top eye hospitals in India. While individual preferences may vary, our commitment to advanced technology, skilled professionals, and patient-centric care has positioned us as a trusted name in eye care.
ASG Eye Specialist Hospital offers a comprehensive range of eye care services, including cataract eye surgery, glaucoma management, retina services, pediatric ophthalmology, neuro-ophthalmology, corneal transplant, refractive surgeries, LASIK surgery, and other eye-related services.
We accept various insurance plans to make eye care accessible to many individuals. Our payment options include cash, credit/debit cards, and several health insurance plans. For specific details, please contact us at 1800 1200 111.
At ASG Eye Hospital, our approach to patient care is delivering personalized and comprehensive eye care solutions. We prioritize patient comfort, employ cutting-edge technology, and ensure our highly skilled medical professionals offer the best treatment options tailored to individual needs.
Yes, you can visit ASG Eye Hospital without an appointment.
Yes, ASG Eye Hospital provides a range of non-surgical options for vision correction. Our experienced optometrists can guide you through options such as eyeglasses, contact lenses, and other advanced vision correction technologies to suit your preferences and lifestyle.
Scheduling an appointment is easy. You can book an appointment through our website, call our helpline, or visit our ASG Eye Hospital locations. Our friendly staff will assist you in selecting a convenient time for your consultation with our experienced eye specialists. Schedule an appointment through our website or call our toll-free number: 1800 1200 111 to book an appointment.
ASG Eye Hospital is recognized among India's top 10 eye hospitals, offering comprehensive eye care services with a team of skilled specialists and advanced treatment facilities.
To find the best eye clinic near you, browse the best eye specialist clinic near me and conduct an online search, check the reviews of websites, consult local directories, ask for recommendations, and consider seeking advice from your primary care physician.
Dr. Arun Singhvi and Dr. Shilpi Gang are the Co-founder, Chairman, and Managing Director of ASG Hospital Private Limited (ASG) which today boasts a geographically diversified presence with 165+ specialized eye hospitals across 83+ cities in India and two international hospitals, each in Uganda and Nepal.